Thousands of Colorado patients put in peril due to risky prescribing of psych medicine

Gene Estes implored his son, Shayn, to go to the emergency room that day, fearful he was having another reaction to his psychiatric medication. Shayn was forgetful, dropping things throughout the day, combative and disoriented during simple conversations.
“I wanted him to see any doctor available,” Estes said.
Gene was worried the dosage was off again. But Shayn, 33, brushed off his father’s concerns as an overreaction. He jumped out of the car after the two argued at the post office and took off walking the six blocks to his Crested Butte apartment.
That was the last time the father would see his son alive. He found Shayn the next morning, on Oct. 17, 2020, dead in his bed, lying on the top of the sheets, still clothed.
Nearly six months after Shayn’s death, a psychiatrist at Mind Springs Health, the community mental health center that runs West Springs Hospital, the Grand Junction psychiatric hospital where Shayn sought psychiatric care, filed a complaint with a state oversight contractor alleging potentially fatal prescribing of benzodiazepines at West Springs and potential harm to patients like Shayn.
An investigation into those claims by the state contractor, Rocky Mountain Health Plans, would eventually force the resignation of Dr. Thomas Newton, another psychiatrist at West Springs. Newton resigned in May 2021 after an investigation found he engaged in “aberrant prescribing” of benzodiazepines – the same drug he had prescribed Shayn Estes. It’s a drug the father now suspects caused his son to fatally overdose while sleeping, though he has no definitive answer.
“If Hippocrates could be found, he’s probably rolling around in his grave,” he said, referring to the ancient Greek physician credited with the Hippocratic Oath, which is still voiced today: “First, do no harm.”
'A broken system'
The heavy reliance on benzodiazepines at Mind Springs has been alarmingly common in Colorado, with state reports identifying thousands of patients as at potential lethal risk because of unsafe prescribing practices, an investigation by The Gazette has found. Known as “benzos,” the anti-anxiety drugs include trade names like Klonopin, Valium, Xanax, Ativan and others, and they are soaring in popularity.
Even as state officials are seeking to rein in the use of benzodiazepines, prescriptions for the drugs nearly doubled over the past two years during a time when the COVID-19 pandemic battered psyches, said Dr. Robert Valuck, executive director of the Colorado Consortium for Prescription Drug Abuse Prevention, housed at the University of Colorado Anschutz Medical Campus.
“These are now the most commonly prescribed controlled substances in Colorado,” Valuck said.
Medicare prescribing data show that 98 practitioners in Colorado had a single year in which they had a higher volume of prescribing benzodiazepines than Newton in the years between 2013 and 2019. Of those, 1 in 5 had their medical license sanctioned by the Colorado Medical Board, and the board cited nearly a dozen specifically for risky benzodiazepine prescribing.
The Gazette also found heavy prescribing of benzodiazepines to Colorado nursing home residents, despite benzodiazepines putting the elderly at increased risk of disorientation, falls and broken bones. One doctor who worked for one of the top prescribers of benzodiazepines to nursing home residents in Colorado said he saw nursing homes he worked with use the drug to cover up staffing shortages and to inappropriately sedate restless residents.
“It’s a broken system,” said Dr. Hugh Batty, now retired and living in Sheridan, Wyo., referring to what he termed excessive reliance on benzodiazepines he said he saw in nursing homes in Colorado.
Doctors who heavily prescribe benzodiazepines say the benefits outweigh the risks. The drugs are popular, because they quickly quell severe panic attacks and help with seizures and insomnia. But studies have found them to be addictive and disorienting, especially in the elderly, who are at increased risk of falls and fractures when they take them. Benzodiazepines also increase the risks of overdose when taken with opioids, alcohol or other drugs that can suppress breathing.
The U.S. Food and Drug Administration has placed a black-box warning, the most serious label from the agency, on benzodiazepines. The warning cautions that benzodiazepines significantly increase overdose risk when combined with opioids, and that they can also lead to physical dependence, addiction and misuse.
Benzos were among the 10 drugs found in the body of Foo Fighters drummer Taylor Hawkins, who died in March in a Bogota, Colombia, hotel room.
A 2013 study by the Centers for Disease Control and Prevention found that benzodiazepines were involved in about one-third of the fatal narcotic overdoses nationwide in 2010.
“Typically, where you run into challenges is when you combine anything else that can depress the central nervous system, like opioids or alcohol, with benzodiazepines,” said Dr. Christopher Jones, who co-authored the CDC study and is the acting director of the agency’s National Center for Injury Prevention and Control.
Another 2019 CDC study found benzodiazepines were involved in about a quarter of overdose deaths due to kratom, an herbal extract that is unregulated and requires no prescription that can also suppress breathing.
Despite the risks, state officials have found widespread reckless prescribing of benzodiazepines by Colorado doctors.
The Colorado State Auditor’s office reported last year that in 2018 and 2019 nearly 13,000 prescribers in the state prescribed a benzodiazepine to a patient already prescribed an opioid from a different prescriber. Nearly 18,000 prescribers ordered an opioid for a patient with a benzodiazepine prescription from a different prescriber in those years, the audit found.
The audit also found that during those years, the 20 prescribers who created the most prescribing volume for such dangerous drug combinations in Colorado allowed nearly 3,000 patients to obtain more than 13,000 concurrent prescriptions of benzodiazepines and opioids.
The Colorado Department of Health Care Policy and Financing, which runs the state’s Medicaid program, reported to federal regulators that it similarly found benzodiazepines were “widely prescribed” in 2018 with other drugs in Colorado, despite evidence that shows doing so is a major risk that leads to “increased central nervous system depression and respiratory depression.”
Valuck, the executive director for the Colorado Consortium for Prescription Drug Abuse Prevention, said recent data show Colorado prescribers are doing a better job of ensuring opioids and benzodiazepines aren’t prescribed in tandem. So far this year, about 6% of patients in Colorado were co-prescribed opioids and benzodiazepines, down from 14% two years ago, Valuck said.
“People who are writing opioid prescriptions are changing,” he said. “The co-prescribing is starting to drop this year.”
A father mourns
Newton heavily prescribed the benzodiazepine alprazolam, which goes by the trade name Xanax, for Shayn Estes, according to prescriptions provided by Shayn’s father, Gene, and reviewed by The Gazette. Gene Estes blames the benzodiazepines for the death.
“The prescriptions he was on left him pretty strung out,” Gene Estes said. “I would put it to the medication.”
Shayn Estes’ autopsy concluded that he probably died from an accidental overdose of kratom, though benzodiazepines prescribed by Newton were also among the drugs found in his body. The autopsy also stated that bottles of prescribed opioids, along with other medications for anxiety and depression, were found in Shayn Estes’ apartment, where the father found his son’s body.
Shayn struggled with epilepsy, which caused him to have seizures, and attention deficit hyperactivity disorder. He was in and out of West Springs Hospital in Grand Junction, where Newton treated him, according to his father.

Shayn had struggled with his psychiatric medications before, Gene Estes said. Once, four months before Shayn fatally overdosed, an air ambulance had to take Shayn to St. Mary’s Medical Center because he was having trouble breathing, the father said. That time, doctors warned that Shayn was on double the normal dosage, according to the father.
Newton and officials with Mind Springs did not respond to requests for an interview. Mind Springs officials in response to earlier articles said in written statements that they have put in place a 17-point corrective action guide demanded by Rocky Mountain Health Plans that will limit and put new oversight over the prescribing for Mind Springs patients. RMHP is the private company that the state’s Medicaid program contracts to oversee Medicaid benefits on the Western Slope.
Gene, now 81, was 45 when Shayn was born. Shayn’s mother died when Shayn was 7. Gene and Shayn Estes were close and saw each other daily.
“He was virtually my only life, particularly from the time his mother died,” Gene Estes said.
Shayn, who took up photography at age 14, turned down a scholarship to study photography at the Savannah College of Art and Design in South Carolina that he was offered after winning second place in a local art contest. Gene Estes remembers Shayn saying he couldn’t take the scholarship because it would mean he would have to leave the mountains of Colorado, which he climbed and hiked every chance he got.
“He was on top of every single mountain in the valley at least once,” the father said. “There’s no place I can go from Crested Butte to Grand Junction that there aren’t memories along the way.”
He still hasn’t had the emotional strength to go through the more than 6,000 photos, many of them of scenic wilderness, that Shayn had taken. A high school friend of Shayn’s put all the photos on a thumb drive and left it for Gene so he could look at his son’s work when he is ready.
“I haven’t gone through them because of the emotion,” Gene said. “I’m getting to where I can. I’m getting to a point where I can start thinking about doing it.”
'Holy Trinity' prescribed to addict
Heavy prescribers of benzodiazepines sanctioned by the state medical board include Dr. Andrew Ho, who practiced internal medicine in south Denver. He prescribed what addicts on the street call the “Holy Trinity,” a dangerous combination of muscle relaxants, opioids and benzodiazepines, court documents show. Although the combination is in high demand on the streets, it carries potent dangers, because it depresses the central nervous system and breathing.
One patient told investigators Ho repeatedly prescribed the “Holy Trinity” drug combination to her at a time when she was addicted and “popping pills like candy.” Even after pharmacists warned Ho to stop the dangerous prescribing, he continued to do so, court documents state.
Ho was sentenced in January 2020 to five years of probation after he pleaded guilty in U.S. District Court to one count of prescribing without a legitimate medical reason in a plea agreement that resulted in the dismissal of 20 other criminal charges.
Ho remains licensed as a doctor, though he’s currently barred from prescribing and has been ordered by the Colorado Medical Board to take classes on proper prescribing practices before he can resume giving out prescriptions.
Ho, who did not return messages seeking comment, claimed in court documents that he was naïve and that “it was easier to prescribe medications than to engage in the difficult discussions that could result from conducting the necessary investigation to root out these issues.” Prosecutors argued Ho’s “rationalizations underscore the casual recklessness of the defendant’s serious crime.”
Another facility in Colorado with heavy benzodiazepine prescribing in the data, Springbok Health Inc., a substance abuse treatment center with clinics in Colorado Springs and Pueblo, and its owner, Mark Jankelow, last month agreed to pay between $125,000 to $335,492 to settle a whistleblower claim filed in U.S. District in Denver alleging health care fraud. The settlement, obtained by the U.S. Justice Department, settled allegations of fraudulent billing of Medicare and Medicaid for high-complexity and prolonged medical evaluation and management services never actually rendered. Jankelow did not return messages seeking comment.
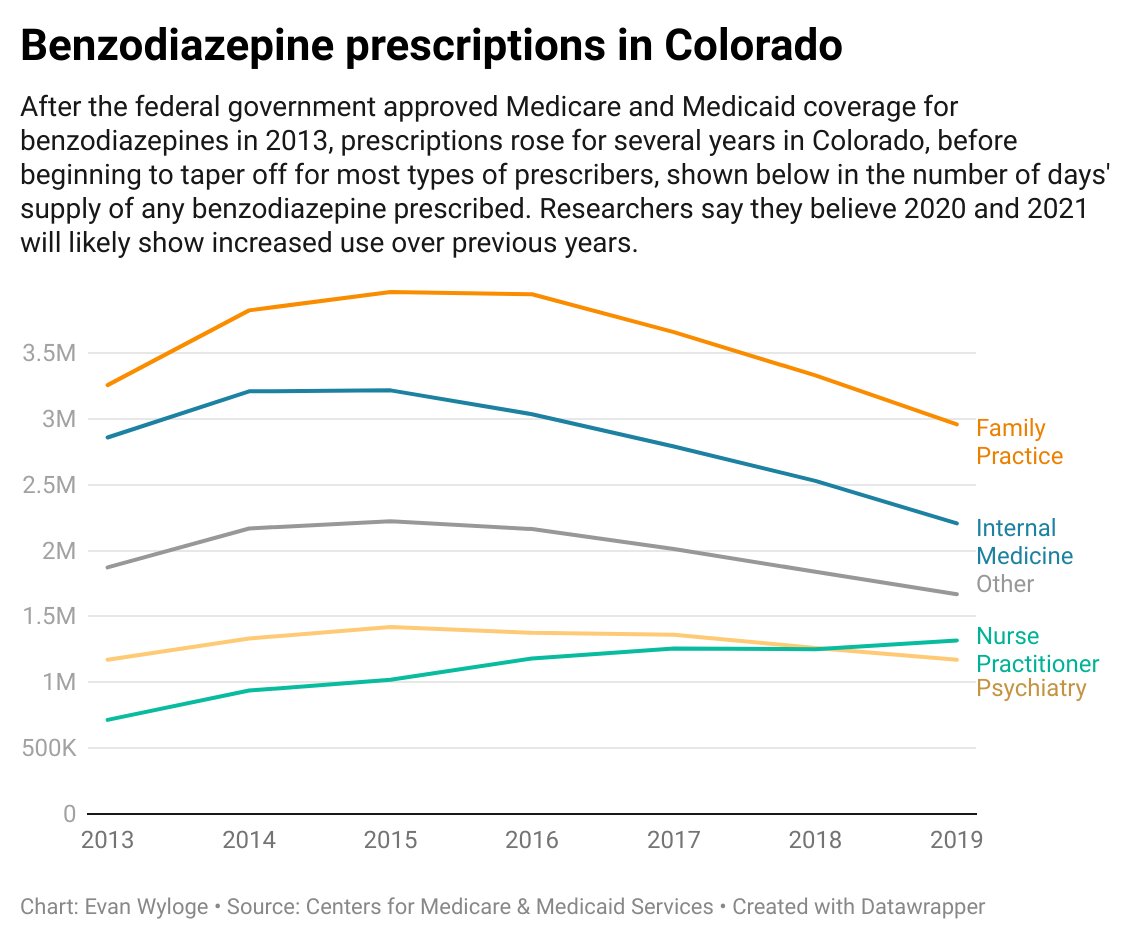
When Congress in 2006 created Medicare’s drug program, called Part D, they decided not to pay for anti-anxiety medications like benzodiazepines. But lawmakers later reversed that payment policy in 2013 under pressure from patient groups and medical societies.
Medicare patients younger than 65 still can qualify for drug coverage due to a disability. Patients with disabilities made up about a quarter of Part D’s enrollees nationwide, but they use benzodiazepines disproportionately, according to studies.
The Gazette analyzed Medicare Part D prescribing data from 2013 through 2019 to identify who prescribed the drug heavily in Colorado during those years. The Medicare data only represents a portion of the prescribing in the state. The Gazette did not have access to data on prescriptions paid by Medicaid or private insurers.
Colorado’s heavy benzo prescribers include Dr. John Hardy, a Pueblo psychiatrist who specializes in child and adolescent treatment. He was among the top 10 prescribers of benzodiazepines in Colorado from 2013 through 2019, prescribing an amount that what would equate to providing more than 960 patients, each, a half year’s supply of the drugs. At a time when others in the top 10 have begun to cut back on their prescribing of benzodiazepines or kept their prescribing consistent, Hardy has increased his prescribing of the drug, the Medicare data show.
Drug companies paid Hardy nearly $900,000 from 2014 to 2020, records show. The drug company payments include consulting and speaking fees as well as travel, lodging and meals.
“I’ve been practicing for many years, and if you stay in the same place, you end up taking care of a lot of people,” Hardy said, denying that drug company pay shapes his prescribing decisions. “I’ve never spoken for a benzodiazepine company.”
Dr. Lora Shirar, a doctor who owns Golden-based Rocky Mountain Senior Care, which provides medical care to more than 650 nursing homes and assisted-living facilities in Colorado, had the highest peak-prescribing year for benzodiazepines in the state, according to the Medicare data. In 2016, she prescribed an amount equal to providing roughly 400 patients, each, a half a year’s supply of the drug, 45% more than the peak year for any other prescriber in Colorado, according to the federal data.
Shirar said she thinks the numbers are inflated, because they may include prescribing by other doctors who work for her business. Since 2016, benzodiazepine prescriptions from her dropped precipitously, down to what would equate to roughly eight patients, each, receiving a half year’s supply of the drug in 2019.
Four other doctors who worked for Rocky Mountain Senior Care had a higher peak year volume of prescribing than any peak year for West Springs’ Dr. Newton for the years analyzed.
The state medical board suspended the medical practice of one of them, Dr. Kurt Wever, in June 2018, when he worked for Rocky Mountain Senior Care, because it found aberrant and dangerous prescribing for four patients in 2011 through 2015.
Three of Wever’s patients — a 45-year-old female, a 48-year-old male and a 62-year-old female — had been taking opioids and benzodiazepines in tandem, documents show. Wever continued prescribing drugs after one patient overdosed and after allegations surfaced another patient was selling morphine, according to medical board documents.
The board also found that Wever didn’t taper drugs, evaluate “medication-induced” seizures in another patient or adequately investigate why another patient’s heart rate soared to 136 while on prescribed medications.
In July 2018, the board reinstated Wever’s license to practice medicine, concluding “that the public health, safety or welfare does not require emergency action at this time.”
Wever did not return telephone and email messages seeking comment. Wever’s prescribing issues occurred years before he worked for Rocky Mountain Senior Care, Shirar said, noting that the medical board had found no ongoing danger.
“When the reality of the case was fully disclosed and investigated, there was no concern,” she said.
Shirar said she and other doctors at her business take precautions when prescribing benzos for nursing home residents. She said there are monthly reviews in nursing homes to monitor prescribed medications.
“There is a check and balance,” she said. “And there is a balancing in the system where patients have rights and need to be engaged as long as possible. They have to have decision making. You can’t just stop everything. Sometimes you have to taper them off and get patient engagement. You have to respect their ability to make decisions.”
But Hugh Batty, who worked for Shirar’s business for two years, said he saw widespread misuse of benzodiazepines during his time in Colorado due to staffing shortages in nursing homes.
“It’s just a pervasive problem,” Batty said of the use of benzos he saw at the facilities where he worked. “The nursing home structure is broken. It’s one of the greatest liabilities we have in our society. People have just jumped in to make money.”
He said doctors like him and Shirar try to limit the use of benzodiazepines for nursing home residents, but nursing home administrators want them prescribed heavily because they don’t have enough employees to monitor residents. The benzos sedate residents and make them easier to control, Batty said. The nursing home administrators will fire doctors if they don’t go along, he said.
“The patients don’t have enough one-on-one care,” he said. “That’s the problem. In order to make ends meet and address the bottom line in a business model, they go short on staffing in nursing homes.”
“You put them on too many benzos, and they are more at risk of falling. It’s not the prudent practice of medicine,” he said.
“You get someone 85, and you give them Xanax — Christ almighty, unless you have someone on each side of them when they’re walking, they’re going to fall down,” Batty said
He added elderly nursing home residents are prone to broken bones if they fall. “And a broken hip at that age is essentially a death sentence,” he said.
State regulators try to limit use
The heavy use of benzodiazepines in Colorado has generated debate over whether state regulators are doing enough to rein in their use. An audit released by the Colorado State Auditor's Office in 2021 recommended that state regulators and law enforcement be allowed access to prescribing data in Colorado to identify medical practitioners with aberrant prescribing of benzodiazepines.
Regulators in 37 states can access such prescribing data, according to the audit, and 22 other states allow law enforcement access. But Colorado doesn’t allow police to access the data without a subpoena, and regulators in the state can only obtain prescribing data after a complaint is filed against a prescriber.
The Colorado Department of Regulatory Agencies is still exploring whether easing access to the data could be a solution, though that’s unlikely to happen, given all the pushback from doctors and patients who fear intrusions on patient privacy, Valuck said.
The Legislature is also considering ways to encourage more doctors to use Colorado’s Prescription Drug Monitoring Program. State law requires prescribers to use the program to check a patient’s prescription history to ensure a patient isn’t taking other drugs, such as opioids, which enhance the risks of prescribing benzodiazepines. Despite that law, a 2021 audit from the Colorado State Auditor’s Office found that 18% of prescribers in Colorado aren’t even registered to use that program.
House Bill 22-1115, sponsored by Rep. Cathy Kipp, D-Fort Collins, and Matt Soper, R-Delta, requires the state to spend $2 million to reimburse doctors and pharmacists who integrate the PDMP prescribing check system with their electronic medical records. Supporters of the legislation, which passed the Legislature and is awaiting signature by Gov. Jared Polis, say ensuring prescribing history checks are done automatically would save time for practitioners who balk at doing the checks manually because they say doing so takes too much time.
In February 2021, Colorado’s Department of Health Care Policy and Financing required prior authorization from state officials before a medical practitioner can bill Medicaid for prescribing benzodiazepines in excess of 90 days for patients 65 years or older.
The agency in 2019 previously put in place prior authorization for Medicaid patients taking opioids long-term and receiving a new prescription for benzodiazepines and vice versa.
Legislation passed last year also requires licensing boards for medical practitioners in Colorado to create new rules limiting how many days a benzodiazepine can be prescribed to patients not already prescribed the drug, with exceptions allowed for patients with severe disorders and neurological conditions.
One patient’s fight
Even with the new laws and regulations, Colorado needs to do more to ensure benzodiazepines are properly prescribed, said one former chronic user of the drug who contends benzos diminished her health for years.
Terri Schreiber, who runs the Schreiber Research Group, an advocacy group seeking to limit benzodiazepine prescribing, said the state needs to make sure patients prescribed benzodiazepines are signing consent forms that warn them of the risks. She said the state also needs to do a better job of identifying heavy prescribers of the drug and educating them of the risks of heavy use.
Schreiber said she struggled with chronic back pain and severe insomnia that only became exacerbated when she sought out medical help more than 20 years ago. She was prescribed benzodiazepines in 2001. Then six years later, while still prescribed benzodiazepines, she received a new prescription for opioids. She took combinations of the drugs for a decade before realizing at age 54 that they were harming her health. The doctors who prescribed the drugs never warned her of the dangers, she said.
“I became disabled from the medication,” Schreiber said. “I had to use a walker. And I became bedridden. I said, ‘I’m too young for this. This cannot be my destiny.’”
An allergist and a pharmacist in 2016 helped her to taper the use of the drugs until she was able to eventually stop using them completely. She said she struggled with withdrawals for 18 months. She could only sleep two to four hours a night and struggled with heart palpitations and a sore throat.
Now, she’s gotten over those side effects and manages her pain through massage, diet, exercise and by practicing mindfulness. She said she no longer must use a walker and doesn’t languish long hours in bed.
“I’m very lucky,” she said. “Very lucky. The fact was that I didn’t know what was happening or how I was at such a high risk until the public figures started to die, and then I started asking questions.”